18th January 2019 marks nine years since I was diagnosed with HIV at 24 years old.
I remember the day of my diagnosis vividly. From my arrival at the STI clinic, the nurse leaning forward and touching my leg gently as she told me that I was HIV positive, to the walk back to my apartment afterwards or confiding in my friend Joe, the first person I told about my HIV status. All of these are moments I will never forget.
In the intervening nine years, the medical approaches to HIV have changed dramatically – and so has my life.
The first year after my diagnosis was the hardest. Within two weeks I had told my 12 closest friends. However, I did find it difficult to speak about my HIV more widely. I grasped that I could anticipate a normal lifespan, but at this stage I could not imagine telling my employer or parents. I felt guilt, shame and fear. I was sometimes so unhappy that I even contemplated taking my own life. My biggest regret from this period is not reaching out to access peer support. I needed to speak to other people living with HIV and attending a newly diagnosed peer support group would have been hugely beneficial.
I am now an HIV activist and writer. Between 2010 and the end of 2012 I came to terms with my HIV diagnosis and, from 2013, I started to look outwards. I was working as a lawyer and hosted several Supper Club dinners for the Terrence Higgins Trust to raise funds for other people living with HIV. As I became involved with HIV activism, I realised that this was where my real passion lay.
I was fortunate to be offered a column with The Huffington Post in 2014, where I reflected on a life living with HIV. I speak out on a range of human rights issues, although HIV, hepatitis C, LGBTQ issues, homelessness and faith inclusion remain at the core of my message. I left my career as a lawyer to become a full-time activist in 2015. I now write for many different publications, including Gay Times. Gay Times have always been at the forefront of LGBTQ and HIV campaigning, so I am pleased to be a part of that tradition.

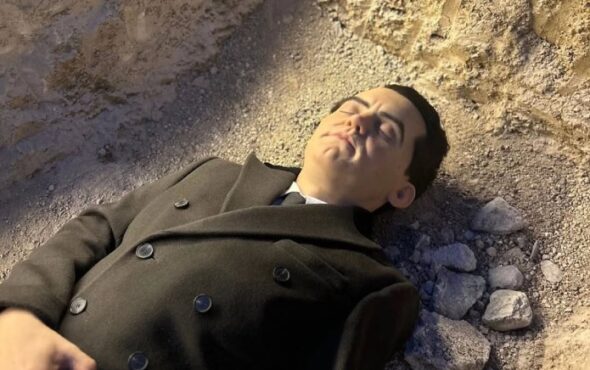
Philip Baldwin
Related: HIV diagnoses are falling in the UK, but this is no time for complacency
I visit schools as a Stonewall Role Model, discussing coming out and faith. I am working on a semi-autobiographical book on stigma called Positive Damage. My metamorphosis from terrified patient to outspoken activist took a number of years, but I am now more empowered and happier than I have been at any other time in my life.
The medical situation around HIV has also changed dramatically. When I was diagnosed with HIV, NHS policy was to advise patients to wait to commence treatment until their CD4 count, a measure of white blood cells, had fallen to between 300 and 500. CD4 cells fight infection and a normal range is said to be between 500 and 1,500.
I did not start HIV medication until December 2012, my CD4 count falling significantly between September and December 2012. The START trial, the results of which were released in 2015, showed decisively that patients should commence treatment as soon as possible following their diagnosis, reducing the capacity for the virus to damage the immune system.
Furthermore, studies such as PARTNER and PARTNER 2, have shown that once an HIV positive person is on effective treatment they can’t pass it on. Commencing treatment as soon as possible after diagnosis not only protects the patient, but prevents onwards transmission.
Equally revolutionary has been the emergence of Pre-Exposure Prophylaxis (PrEP). PrEP is a drug taken by HIV-negative people that prevents the transmission of HIV. On two occasions prior to my HIV diagnosis in 2010, I had taken Post-Exposure Prophylaxis, a combination of HIV medications which, if administered within 72 hours of exposure, can prevent the HIV virus from taking hold. It was not until 2014/2015 that PrEP started to become available privately in the UK, but had it been available in 2010 I might not be HIV positive today.
It is a particularly exciting time for PrEP, with NHS England recently endorsing a recommendation for places on the PrEP IMPACT Trial to be doubled from 13,000 to 26,000. However, this is not yet a done deal and it’s vital all players involved in the trial act quickly to make this happen. Over 40 clinics in the UK have had to turn gay and bisexual men away, as they were at full capacity. We know that a number of these men have gone on to become HIV positive.
It is welcome news that the IMPACT trial is potentially increasing places, but I want to use the ninth anniversary of my HIV diagnosis to repeat the call for PrEP to be made routinely available on the NHS to all who could benefit from it. Every HIV diagnosis is preventable.
Click here to learn more about the work of the Terrence Higgins Trust.
Related: 5 key goals we need to focus on in 2019 to reduce HIV diagnoses